Introduction
Despite major progress in antimicrobial and supportive measures, prolonged disease-associated or treatment-related neutropenia is a leading cause of mortality and morbidity in patients after stem cell transplantation or with hematologic malignancies or bone marrow failure. Intuitively, a granulocyte transfusion should be as effective as a platelet or red cell transfusion. However, efforts to prove the effectiveness of granulocyte transfusions have been disappointing. Due to the lack of adequately powered randomized controlled trials, it is difficult to prove or refute the effectiveness of granulocyte transfusions in neutropenic patients. Therefore, they are likely underutilized or used inappropriately as a last resort. To better understand the utility of this treatment modality, we reviewed the outcomes of patients with hematologic conditions who received granulocyte transfusions at our institutions during the treatment of neutropenic sepsis.
Methods
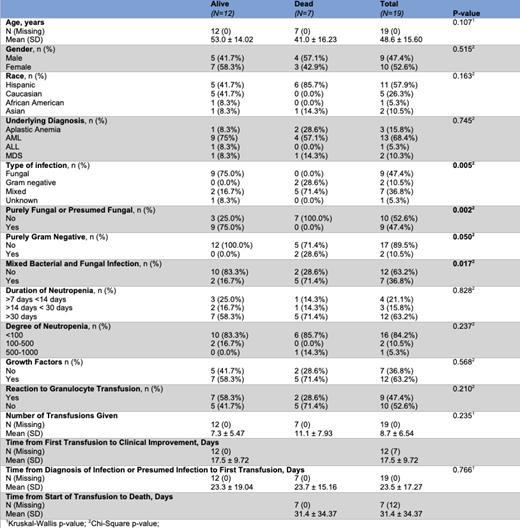
We identified 20 patients with severe neutropenia who received a granulocyte transfusion at Norris Comprehensive Cancer Center or Keck Hospital of USC in Los Angeles, California between 2014-2022. 19 of these patients received a total of 166 transfusions for treatment of suspected or confirmed sepsis. One patient received a prophylactic dose of granulocytes and was excluded from this study. Granulocyte donors were mobilized with 480 mcg G-CSF and a minimum yield of 4 x 10 10 granulocytes was obtained. The primary outcome was attainment of “clinical improvement” defined as either safe discharge from the hospital or resolution of symptoms. Descriptive statistics were presented as counts and percentages for categorical variables and as means with standard deviations for continuous variables. Categorical variables were accessed by Chi-square test or Fischer's exact test when appropriate. For continuous variables, Kruskal-Wallis test was used. P-values of ±0.05 were regarded as significant and all tests were two-tailed and analyzed with SAS (9.4).
Results
In our cohort, 47.4% were male, ages ranged from 20-70, and 57.9% identified as Hispanic. The most common diagnosis was acute myeloid leukemia (AML) (n=13), followed by aplastic anemia (n=3), myelodysplastic syndrome (MDS) (n=2), and acute lymphoblastic leukemia (ALL) (n=1). The most common infections were fungal or presumed fungal (n=9) and mixed fungal and bacterial (n=7). Prior to the start of granulocyte transfusions, 63.2% of patients were neutropenic (ANC <500) for at least 30 days and 84.2% had an absolute neutrophil count (ANC) <100. In surviving patients, the average number of days from the first transfusion to clinical improvement was 17.5 days. 47.4% of patients had a reported reaction to the granulocytes, with the most common being fever and tachycardia.
Of the 19 patients treated, seven (37%) died from infection. Of those who died, two (29%) died from E. coli bacteremia and five (71%) from mixed bacterial and fungal sepsis. All nine patients with acute fungal infections without concomitant bacterial infections survived.
Conclusion
In this cohort, granulocyte transfusions appear to have had a positive effect with 63% of critically ill patients attaining clinical improvement from infection. All patients who had a purely fungal infection achieved clinical improvement and all patients who died had bacterial or mixed infection. Time to transfusion from initial infection, number of transfusions, and demographic variables did not appear to impact overall survival. Granulocyte transfusion could be an effective therapeutic modality in the treatment of infection in patients with prolonged severe neutropenia, especially those with fungal infections. Adequately powered randomized controlled trials are the next step in determining the effectiveness of this treatment.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal